- Introduction :
- Anatomy of Pleura :
- Layers of Pleura :
- The Pleural Cavity :
- Pleural Fluid :
- Blood Supply, Lymphatic drainage & Innervation :
Introduction :
The lungs are enveloped and protected by a thin, serous membrane called the pleura. This membrane plays a crucial role in cushioning the lungs and facilitating smooth, frictionless breathing.
Anatomy of Pleura :
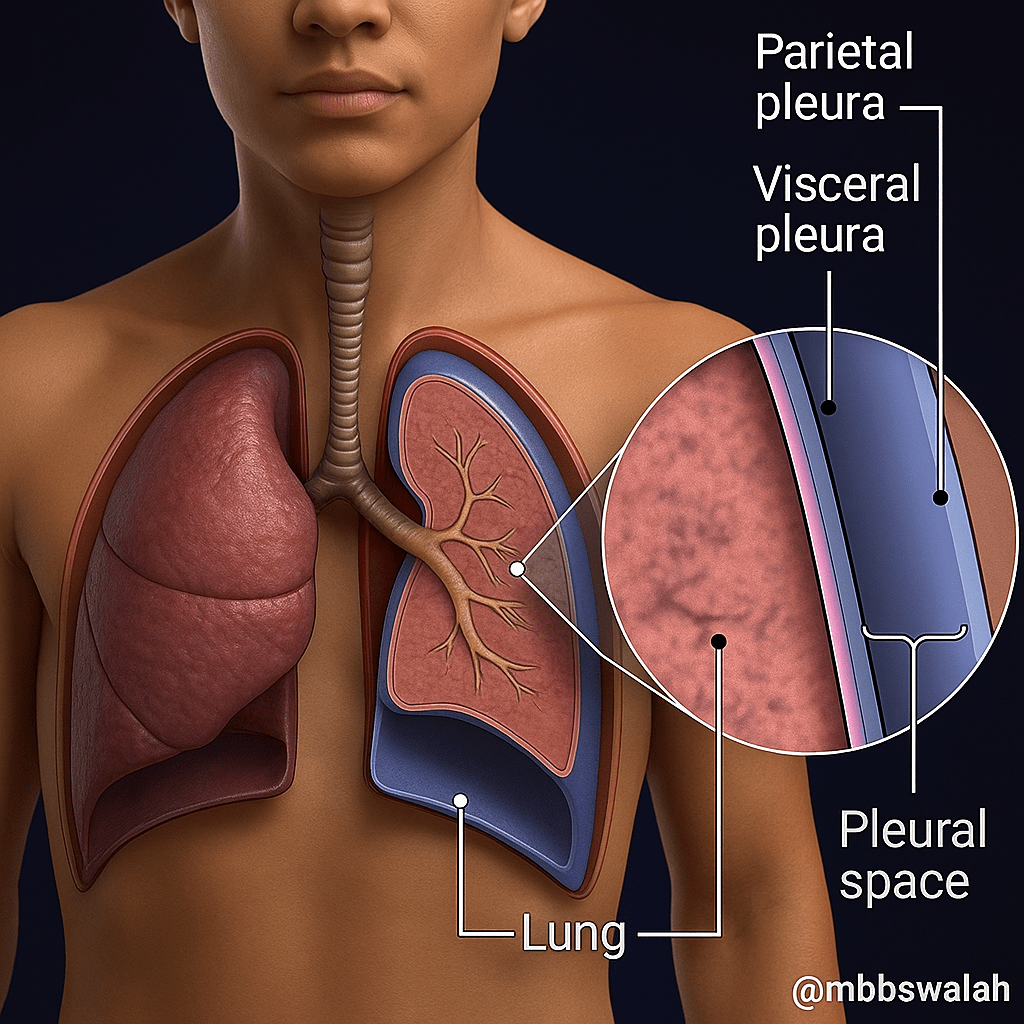
Layers of Pleura
Pleural cavity and fluid.
Layers of Pleura :
The pleura comprises two continuous layers :
Visceral Pleura
Parietal Pleura
Visceral Pleura :
Definition: Inner layer of pleura covering the lung parenchyma.
Coverage: Envelops lungs, including fissures (oblique & horizontal), vessels, bronchi, and nerves.
Lung Lobes: Folds into lung fissures, forming lobes.
Thickness: Thinner and more delicate than the parietal pleura.
Innervation: No sensory nerve supply — insensitive to pain.
Stimuli Sensitivity: Responds only to stretch, not pain.
Parietal Pleura :
Definition: Outer layer of pleura lining the inner surface of the chest wall.
Coverage: Lines thoracic wall, mediastinum, and diaphragm.
Structure: Thicker and more robust than the visceral pleura.
Innervation: Richly supplied with somatic afferent nerves.
Sensitivity: Susceptible to pain, pressure, and temperature.
The parietal pleura is further subdivided based on the specific region of the thoracic cavity outlines or approximates:
Cervical Pleura:
Also known as the cupula, this superior most of the parietal pleura extends into the root of the neck, projecting approximately one inch (2.5 cm) above the medial third of the clavicle. It lines the undersurface of the suprapleural membrane.
Costal Pleura:
This extensive portion lines the inner surfaces of the sternum, ribs, costal cartilages, and intercostal spaces. It also lines the sides of the vertebral bodies. This makes it adjacent to the ribs and intercostal spaces.
Mediastinal Pleura:
This subdivision covers the mediastinum. It is the central compartment of the thoracic cavity. This compartment houses vital structures such as the heart, great vessels, esophagus, and trachea. At the hilum, it reflects onto the vessels and bronchi, becoming continuous with the visceral pleura. It uniquely shapes the outer sidewall of the mediastinum, acting as its lateral boundary.
Diaphragmatic Pleura:
This inferior part of the parietal pleura covers the superior(thoracic) surface of the diaphragm.
The Pleural Cavity :
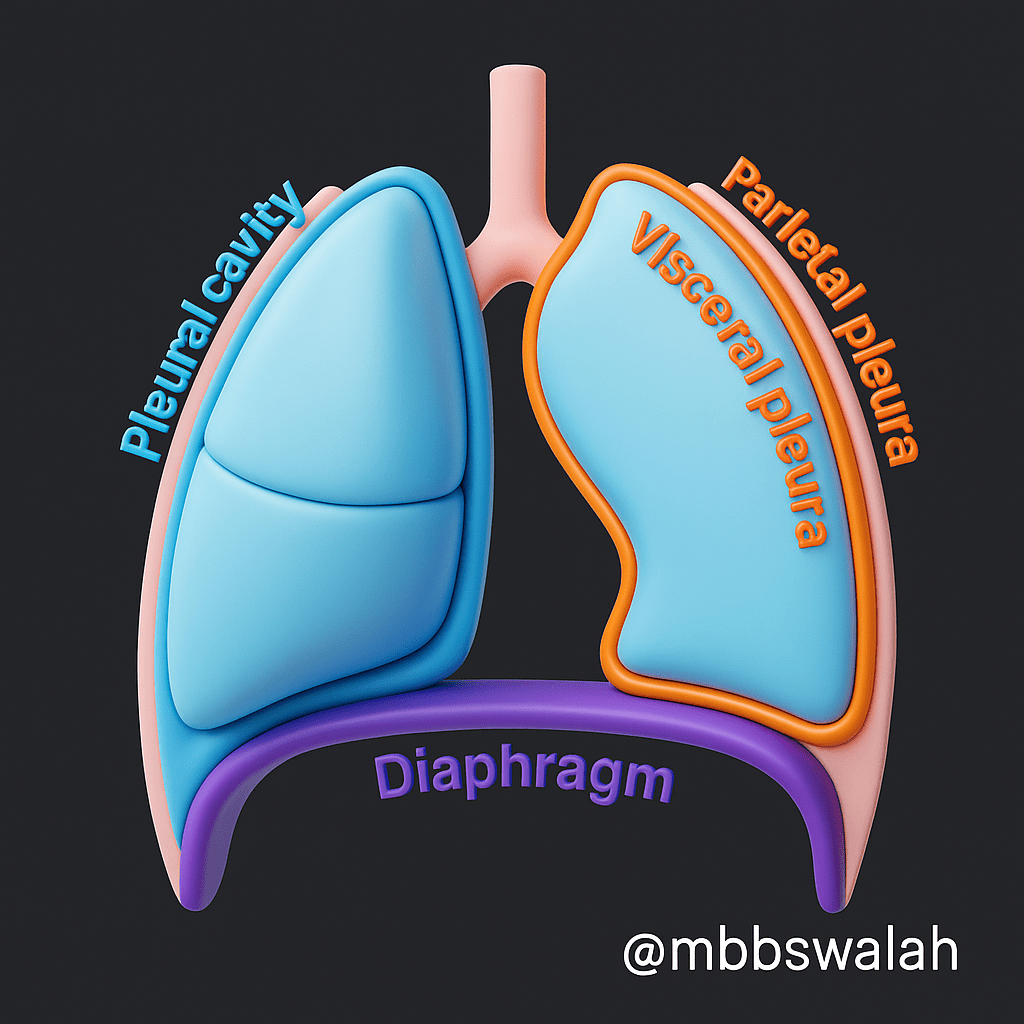
Between the visceral and parietal pleura lies a potential space known as the pleural cavity (pleural space).
In a healthy individual, this space contains only a small amount of serous fluid, typically about 10-20 mL.
Importantly, there is no direct communication between the right and left pleural cavities.
This cavity maintains a negative intrapleural pressure. This is crucial for preventing the lungs from collapsing. It also facilitates their proper function during respiration.
Pleural Fluid :
Pleural fluid is a serous fluid. It is continuously produced primarily by exudation from systemic microvessels. This occurs in the parietal pleura through a process called bulk flow.
Normal Volume: Very small (1–10 ml), essential for proper lung function.
Functions :
Lubrication: Allows smooth, friction-free movement of pleural layers during breathing.
Immune Defense: Contains cells/proteins that help protect against infection.
Surface Tension: Creates negative intrapleural pressure, keeping lungs adhered to the chest wall.
Homeostasis: Balance between production and drainage is critical.
Physiological Role: Dynamic system; even slight imbalances can signal or cause disease.
Blood Supply, Lymphatic drainage & Innervation :
Blood Supply :
The blood supply to the pleura is distinct for its two layers:
Parietal Pleura: This outer layer receives its arterial supply from the systemic arteries that overlie it. These include branches from the internal thoracic artery. There are also anterior and posterior intercostal arteries, the subclavian artery, and the phrenic arteries. Venous return from the parietal pleura occurs similarly, draining into the internal thoracic, intercostal, and phrenic veins.
Visceral Pleura: This inner layer wraps directly around the lungs and gets its blood mainly from the bronchial arteries. Oxygen-rich blood flows back to the heart via the pulmonary veins.
Lymphatic Drainage :
Lymphatic drainage from the pleural cavity primarily involves the parietal pleura.
The parietal pleura contains numerous small openings known as stomata. These openings facilitate the drainage of pleural fluid into the subpleural lymphatic system.
These lymphatic vessels then drain into various lymph node stations. This includes the diaphragmatic, internal mammary, retrosternal, paraesophageal, and celiac lymph nodes.
Innervation :
The nerve supply to the pleura also differs between its layers, directly correlating with their respective pain sensitivities:
Parietal Pleura: This outer layer is very sensitive and can feel pain, pressure, heat, and touch clearly.
The costal pleura is segmentally innervated by branches from the intercostal nerves, which run parallel to the ribs.
The mediastinal pleura mainly gets its nerve supply from the phrenic nerves.
The diaphragmatic pleura is innervated centrally by the phrenic nerves and peripherally by the lower six intercostal nerves.
Visceral Pleura: Unlike the outer layer, the visceral pleura does not feel pain. Its innervation comes from autonomic fibers originating from the pulmonary plexus, making it sensitive primarily to stretch stimuli.


Leave a comment