- Lung Embryology: Essential Insights into Pulmonary Development
- Early Embryonic Development (Weeks 3-5)
- Stages of Prenatal Lung Development
- Postnatal Lung Development:
Lung Embryology: Essential Insights into Pulmonary Development
Human lung formation is a complex biological process that begins early in embryonic development and is critical for respiratory function. Understanding this process is vital for grasping normal lung function. It is also essential for comprehending congenital lung diseases and exploring regenerative therapies.
Early Embryonic Development (Weeks 3-5)
1. Lung Bud Formation:
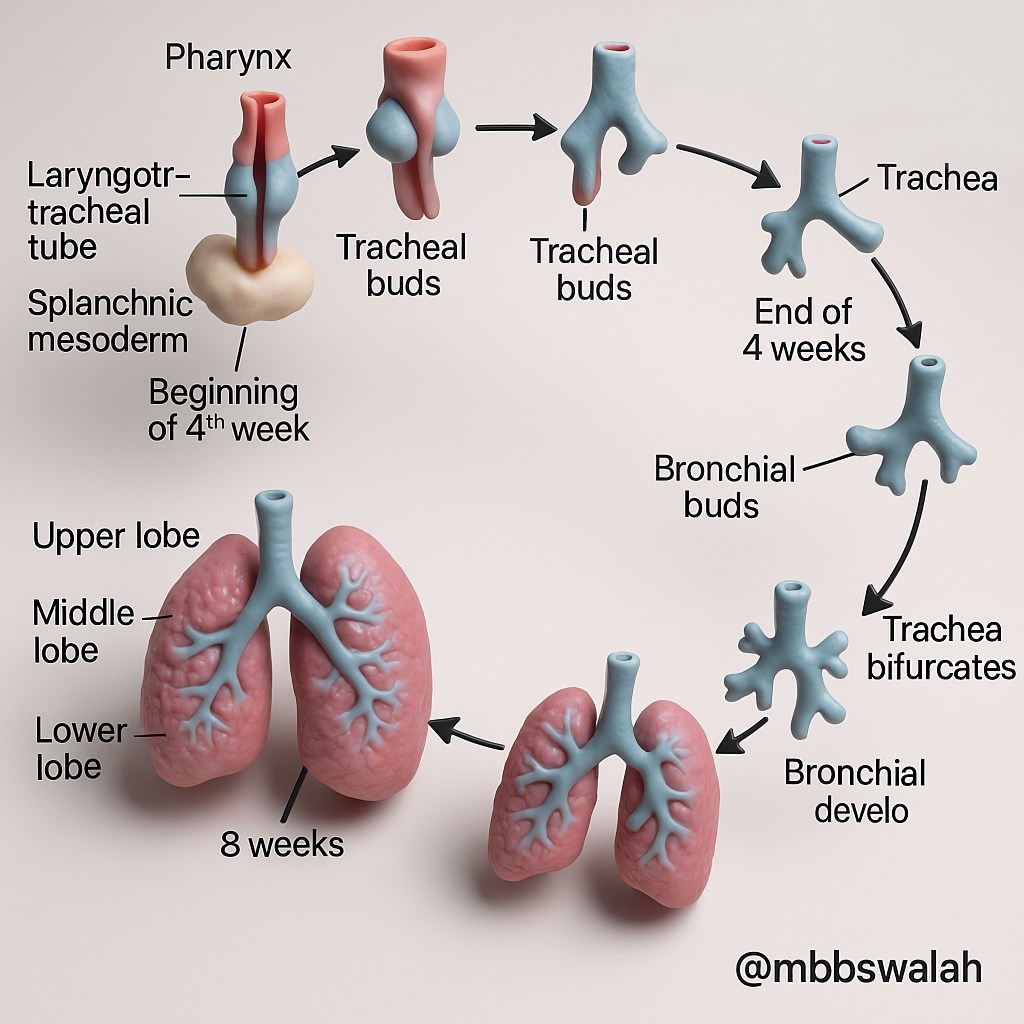
Lung development starts around the late third or early fourth week of embryonic life. At about 26 days, the respiratory diverticulum, or lung bud, emerges from the cranial foregut. This bud will develop into the lower respiratory system, including the larynx, trachea, bronchi, and lungs.
2. Tracheoesophageal Septum Formation:
Initially, the lung bud remains connected to the foregut. In week four, tracheoesophageal folds form, fuse, and separate the trachea from the esophagus. This separation, completed by day 41, is crucial; incomplete separation can lead to serious issues like tracheoesophageal fistulas.
3. Bronchial Budding:
Around day 28, the lung bud bifurcates into two primary bronchial buds. These then branch further to form the lobar structure of the lungs. The right lung develops three bronchi, while the left develops two. This process continues, with secondary bronchi appearing by day 52.
Stages of Prenatal Lung Development
1. Pseudoglandular Stage (Weeks 5-16):
During this stage, lung tissue has a glandular appearance, characterized by branching and the formation of airway structures. By the end of this period, up to 25 generations of conducting airways are formed. Important support structures like cartilage, smooth muscle, and mucous glands begin to develop. However, pulmonary surfactant is not produced. This makes fetuses non-viable if born during this stage.
2. Canalicular Stage (Weeks 17-28):
This stage is marked by the enlargement of bronchi and bronchioles’ lumens and increased vascularity. Developing airspaces begin forming alveoli, and capillary networks approach these spaces. This period sets the stage for the later development of the lung’s gas exchange capabilities.
3. Saccular/Terminal Sac Stage (Week 28 to Birth):
This stage lasts from week 28 until birth. It involves the development of terminal sacs. These sacs are precursors to true alveoli. The epithelium becomes very thin, reducing the diffusion distance for gases. Capillary networks quickly develop, with capillaries bulging into the alveoli. Type I alveolar cells continue to grow. Type II cells significantly increase surfactant production. This increase is crucial to maintain alveolar expansion and prevent collapse. Fetal breathing movements can be detected at this stage. However, only about 8% of adult alveoli are formed by the time of birth, indicating ongoing development postnatally.
Postnatal Lung Development:
Lung development continues after birth through alveolarization and microvascular remodeling, extending into childhood and even young adulthood.
1. Mechanisms of Alveolar Formation (Septation):
Most adult alveoli are formed postnatally. Alveolarization involves subdividing existing airspaces (saccules and ducts) by creating new walls. This process significantly increases the surface area for gas exchange and continues for years, showing substantial developmental plasticity.
2. Microvascular Maturation and Remodeling:
New alveoli formation coincides with microvascular maturation. The capillary network transitions from a double-layered system in the primitive septa. It becomes a single-layered system. This optimizes gas exchange surfaces and minimizes diffusion distances.
3. Transition to Air Breathing at Birth:
At birth, the lungs are filled with fluid. The first breath triggers lung inflation and fluid clearance. Postnatally, lung growth focuses on increasing the number of respiratory bronchioles and alveoli. This growth strategy meets the newborn’s metabolic needs more effectively than enlarging individual alveoli.


Leave a comment