- Introduction :
- What is Atherosclerosis ?
- Stages of formation of ATHEROSCLEROSIS :
- Causes and risk factors :
- Symptoms :
- Diagnosis :
- Treatment options :
- Complications :
Introduction :
Atherosclerosis, a chronic and progressive disease, is characterized by the buildup of plaque within the walls of arteries. This condition represents a major global health challenge, contributing significantly to morbidity and mortality world wide. While often associated with advancing age, the process of atherosclerosis can commence surprisingly early in life, sometimes even during childhood. This early onset underscores the importance of adopting preventive strategies from a young age.
What is Atherosclerosis ?
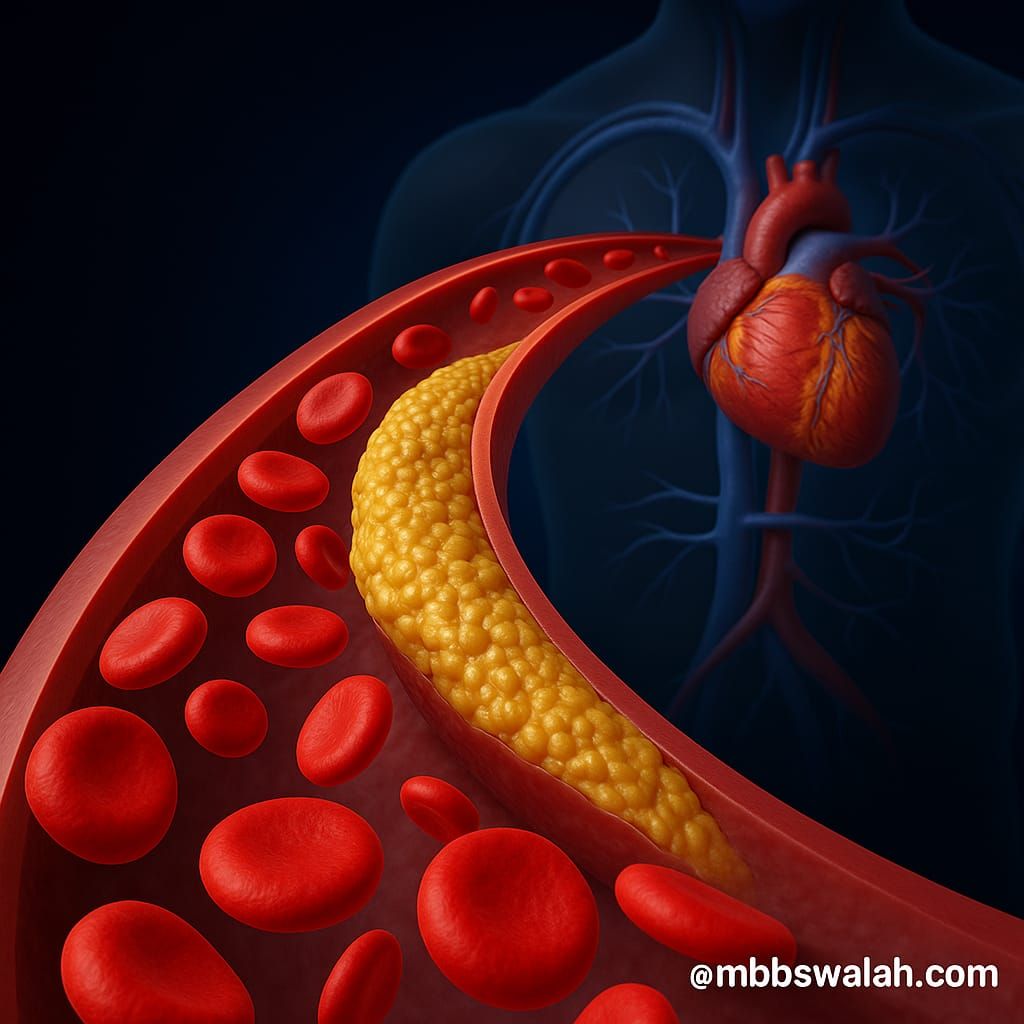
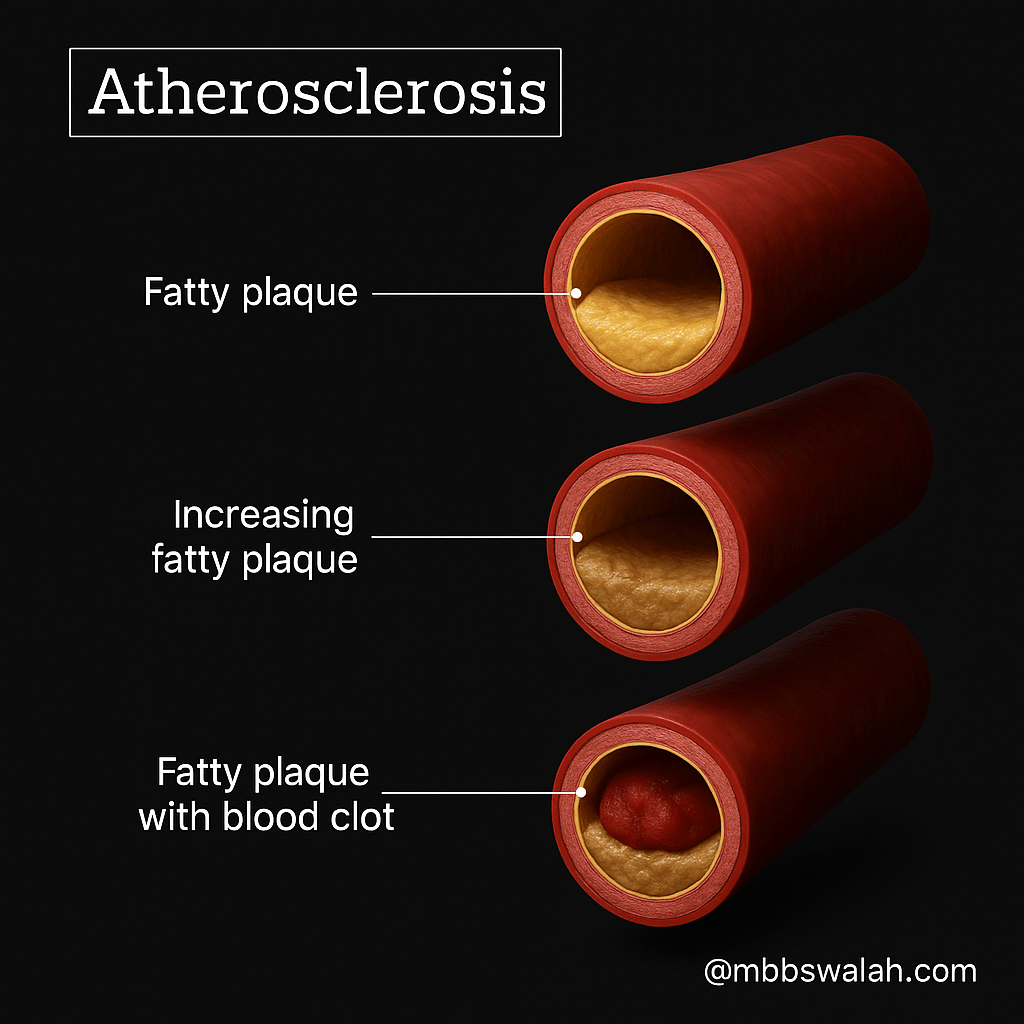
Atherosclerosis is fundamentally defined by the accumulation of plaques inside the arteries. These plaques are complex deposits. They are primarily composed of lipids. This includes cholesterol, fatty substances, cellular waste products, calcium, and a clotting material called fibrin.
Plaques in arteries form through a step-by-step process. The process is mostly driven by fats. A type called LDL (low-density lipoprotein, or “bad cholesterol”) plays a significant role. These fats tend to collect in certain parts of the arteries. They accumulate where blood flow is not smooth, such as at artery branches.
When too much LDL builds up, it can damage the inner lining of the artery, called the endothelium. This damage worsens due to factors like smoking. High blood pressure also contributes to it. High blood sugar from diabetes or more LDL in the blood also worsens it. The damaged endothelium stops producing substances that normally keep blood vessels relaxed. It prevents clots and instead starts attracting white blood cells.
White blood cells called monocytes stick to the damaged area, move inside the artery wall, and change into macrophages. These macrophages “eat” the damaged LDL, becoming foam cells. When many foam cells pile up, they form a fatty streak — the first visible sign of plaque.
As this continues, inflammation increases. More immune cells arrive, and smooth muscle cells from deeper in the artery wall move into the area. These muscle cells help build a cap over the fatty core, forming a fibrous plaque.
This plaque can grow and harden over time. It narrows the artery and makes it harder for blood to flow. This can lead to heart attacks or strokes.
Stages of formation of ATHEROSCLEROSIS :
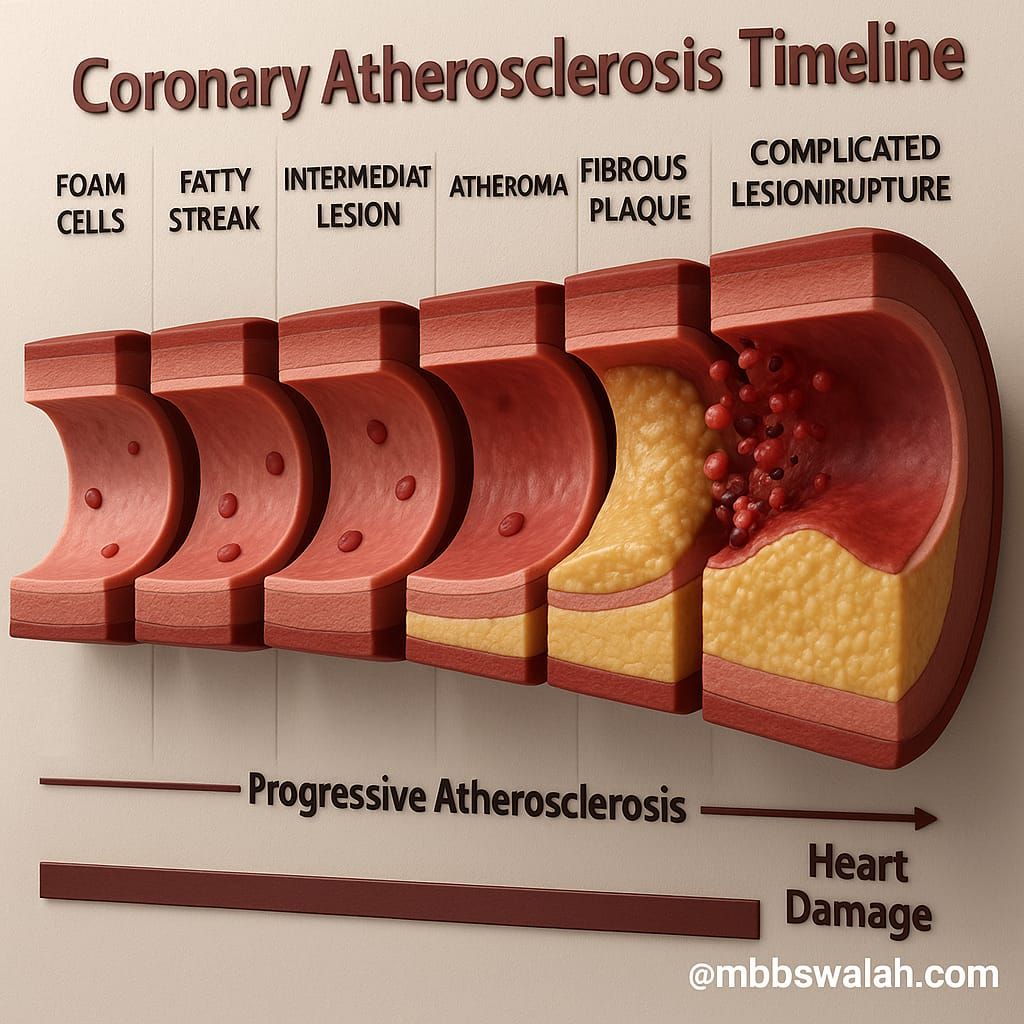
1. Fatty Streak Stage (Early Stage):
- Begins in childhood.
- Modified lipoproteins (like oxidized LDL) accumulate in the inner artery layer (intima).
- Endothelial dysfunction occurs.
- White blood cells (monocytes) stick to the damaged endothelium and turn into foam cells.
- Foam cells form fatty streaks — the earliest visible sign of atherosclerosis.
2. Early Fibroatheroma Stage:
- Smooth muscle cells migrate from the artery’s middle layer to the intima.
- These cells produce collagen, forming a fibrous plaque.
- Lymphocytes (immune cells) join the process and contribute to inflammation.
3 . Advancing Atheroma / Plaque Growth Stage:
- The plaque grows larger.
- A necrotic core (dead cells and lipid buildup) develops.
- More lipids accumulate.
- The fibrous cap becomes thicker.
- Microvessel density increases (small blood vessels grow within the plaque).
4 . Plaque Rupture (Critical Stage):
- The fibrous cap tears (ruptures), exposing inner plaque contents.
- This leads to blood clot (thrombus) formation.
- Common in plaques with a thin cap and lipid-rich core.
- High risk of heart attack or stroke.
5 . Plaque Erosion ( Alternative to Rupture):
- The endothelium (inner lining) is lost, but the fibrous cap stays intact.
- A clot forms without a rupture, usually with less inflammation than rupture.
6 . Necrotic Core Development:
- Lipids from dead foam cells accumulate.
- Intra plaque hemorrhage (bleeding inside the plaque) contributes to core growth.
- This weakens the plaque further and increases the risk of rupture.
Causes and risk factors :
Several factors can initiate damage to the inner lining of the arteries, setting the stage for atherosclerosis. These primary causes include high blood pressure. High levels of cholesterol and triglycerides in the blood are also factors. Smoking and tobacco use contribute as well. Diabetes and insulin resistance play a role. Inflammation arising from various sources is another factor.
The risk factors associated with the development and progression of atherosclerosis can be broadly categorized into modifiable and non-modifiable factors.
Modifiable risk factors are health risks you can change or manage by improving your habits or getting medical help.
Non-modifiable risk factors are health risks you can’t change, like your age, sex, or family history.
| Modifiable risk factors | Non modifiable risk factors |
| Hyper cholesterolemia (high LDL cholesterol) | Age (men >45 years, women >55 years) |
| Hypertension (high blood pressure) | Male gender |
| Cigarette smoking | Strong family history of early heart disease or stroke |
| Diabetes mellitus and insulin resistance | Genetic predisposition and certain genetic mutations |
| Obesity | Inflammatory conditions (lupus, rheumatoid arthritis, psoriasis, (IBD) |
| Sedentary lifestyle/physical inactivity | |
| Unhealthy diet (high in saturated/trans fats,sodium, sugar) | |
| Metabolic syndrome | |
| Sleep apnea | |
| High triglycerides |
Symptoms :
Atherosclerosis often progresses without noticeable symptoms for many years. Manifestations typically appear only when the arteries become significantly narrowed or blocked. The specific symptoms experienced depend on which arteries in the body are affected.
When atherosclerosis affects :
the coronary arteries supplying blood to the heart can cause chest pain or pressure known as angina. It can also lead to shortness of breath. In severe cases, it may result in a heart attack.
the carotid arteries that lead to the brain can cause symptoms that mimic those of a stroke. These symptoms include sudden numbness or weakness in the arms or legs. You might experience difficulty speaking or slurred speech. Other symptoms are sudden changes in eyesight, dizziness, a sudden and severe headache, and drooping muscles in the face. These issues can potentially lead to a stroke or a transient ischemic attack (TIA).
the peripheral arteries, typically those in the legs, atherosclerosis can cause pain when walking (claudication). It can also lower blood pressure in the affected limb. At rest, a burning or aching pain may occur in the feet. Sores can develop on the feet, and in critical cases, it may lead to gangrene.
the renal arteries supplying the kidneys can result in markedly elevated blood pressure that does not respond to multiple medications. It can also cause changes in urination, swelling, fatigue, nausea, and unexplained weight loss.
the intestinal arteries are affected, it can lead to severe abdominal pain after meals, weight loss,and diarrhea.
Diagnosis :
| Diagnostic Method | Principle |
| Physical Examination | Checking for bruits, pulse strength, blood pressure differences |
| Blood Tests | Measuring cholesterol,triglycerides, blood sugar,and inflammatory markers. |
| Electrocardiogram(ECG/EKG) | Measures electrical activity of the heart. |
| Stress Test | Evaluates heart function during exertion. |
| Echocardiogram | Uses sound waves to visualize heart structure and blood flow. |
| Doppler Ultrasound | Checks blood flow speed in arteries. |
| Ankle-Brachial Index (ABI) | Compares blood pressure in ankle and arm. |
| Cardiac Catheterization and Angiogram | Invasive procedure to visualize coronary arteries with dye and X-rays. |
| Coronary Calcium Scan(Heart Scan) | CT scan to detect calcium deposits in coronary arteries. |
| Computed Tomography angiography (CTA) | Uses dye and CT scans for detailed vessel images. |
| Magnetic Resonance angiography (MRA) | Uses magnetic fields to create vessel images. |
| Intravascular Ultrasound (IVUS) | Ultrasound probe on a catheter to view artery walls from inside. |
| Positron Emission | May be used to study |
| Tomography (PET) | Arteries |
Treatment options :
The primary goals of atherosclerosis treatment are to slow down its progression. Treatment also aims to potentially reverse the condition. Preventing serious cardiovascular events, such as heart attack or stroke, is crucial.27 Treatment strategies typically involve a combination of lifestyle modifications, medications, and in more severe cases, medical or surgical procedures.
The selection of the most appropriate treatment strategy depends on the severity of the atherosclerosis. It also depends on the location of the atherosclerosis. Additionally, the patient’s overall health and other risk factors are crucial.
| Treatment Category | Specific Treatment | Description |
| Lifestyle Changes | Heart-healthy diet | Low in saturated / transfats, cholesterol, sodium, sugar; high in fruits, vegetables, whole grains, lean protein. |
| Regular physical activity | At least 30 minutes of moderate-intensity exercise most days of the week. | |
| Weight management | Achieving and maintaining a healthy weight. | |
| Smoking cessation | Quitting smoking and avoiding secondhand smoke. | |
| Moderate alcohol consumption | Limiting alcohol intake. | |
| Stress management | Techniques to reduce stress levels. | |
| Adequate sleep | Ensuring sufficient and good quality sleep. | |
| Medications | Statins | Lower LDL cholesterol levels. |
| Anti-platelet medications (e.g.,aspirin, clopidogrel) | Reduce blood clot formation. | |
| Anticoagulants(e.g., warfarin,heparin) | Prevent blood clotting. | |
| Blood pressure medications | Manage hypertension (e.g.,beta-blockers, ACE inhibitors). | |
| Other cholesterol-lowering medications | Bile acid sequestrants, nicotinic acid, fibrates, PCSK9 inhibitors. | |
| Anti-diabetic medications | Control blood sugar levels in diabetic patients. | |
| Anti inflammatory medications | Reduce inflammation | |
| Catheter-Based Procedures | Angioplasty | Widening narrowed arteries with a balloon-tipped catheter. |
| Stenting | Inserting a mesh tube to keep the artery open after angioplasty. | |
| Atherectomy | Removing plaque buildup from artery wall using a catheter with a blade or laser. | |
| Surgical Procedures | Coronary artery by pass grafting (CABG) | Creating new routes for blood flow around blocked coronary arteries |
| End-arterectomy | Surgically removing plaque buildup from the lining of a blocked artery (e.g.,carotid). | |
| Arterioplasty | Surgical repair of an aneurysm. |
Complications :
If left untreated or advanced, atherosclerosis can lead to a range of serious complications.
- Coronary artery disease (CAD)
- Carotid artery disease.
- Peripheral artery disease (PAD)
- Aneurysms
- Chronic kidney disease
- Mesenteric artery ischemia.


Leave a reply to Anonymous Cancel reply