The thoracic cavity is the chest area that holds the lungs and heart. It is divided into two main regions. The lungs are located in the pleural cavities. The heart and other organs are situated in the mediastinum.
The diaphragm helps with breathing by moving air in and out of the lungs. This area houses and protects many vital organs. Within the middle part of the mediastinum, the pericardium sits. It is a sac that encloses the heart and the roots of its major vessels.
The pericardium’s role is integral within the larger mediastinal compartment, showing a hierarchical organization within the chest. Understanding both is key to thoracic health.
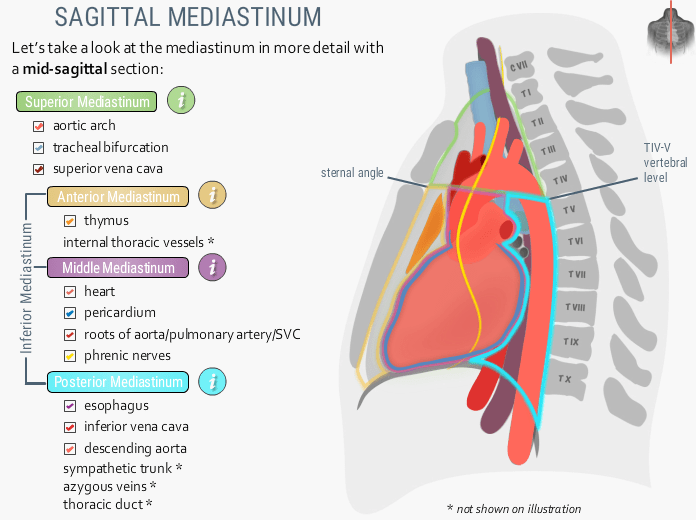
Anatomy of the Mediastinum
Definition & Location:
The mediastinum is the central compartment of the thoracic cavity, located between the left and right pleural cavities. It includes vital structures like the heart, esophagus, and major blood vessels.
Boundaries:
○ Superior: The superior thoracic aperture is also known as the thoracic inlet. It is the opening at the top of the chest. This opening is located at the base of the neck.
○ Inferior: Diaphragm (muscle separating chest and abdomen).
○ Anterior: Sternum (breastbone) and transversus thoracis muscles.
○ Posterior: The thoracic vertebral column forms the posterior boundary of the thoracic cavity. It consists of the T1 to T12 vertebrae in the spine.
○ Lateral: Mediastinal pleura (membranes lining the lungs).
○ These borders are crucial for understanding disease spread. The mediastinum connects to the neck above. It also connects to the abdomen below via the diaphragm.
Subdivisions:
The mediastinum is divided into four main compartments for descriptive purposes. The division between the superior and inferior mediastinum is an imaginary line called the transverse thoracic plane. It runs from the sternal angle (joint between the top and body of the sternum). The front boundary extends from the sternum to the disc between the T4 and T5 vertebrae.
Superior Mediastinum:
Located above the transverse thoracic plane.
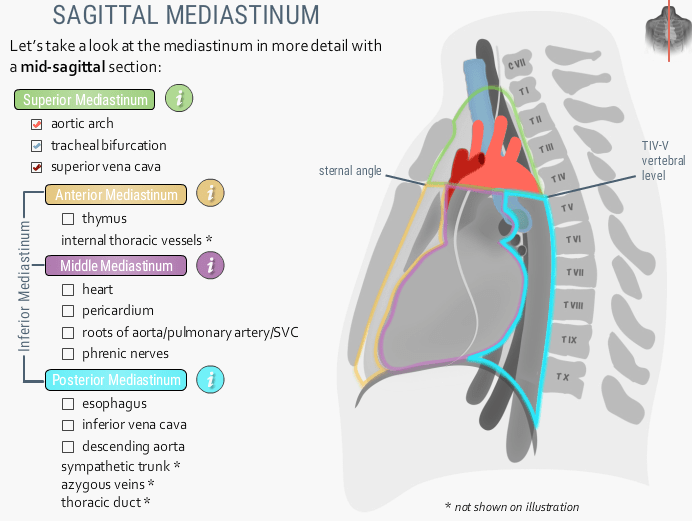
■ Borders: Thoracic inlet (top), transverse thoracic plane (boom), manubrium of sternum (front), T1-T4 vertebrae (back), mediastinal pleura (sides).
■ Contents:
The thymus gland, upper trachea, and upper esophagus are included. The aortic arch and its main branches (brachiocephalic trunk, left common carotid artery, left subclavian artery) are part of it. There are also the upper superior vena cava, brachiocephalic veins, and the arch of the azygos vein. Other components include the thoracic duct, phrenic nerves, and vagus nerves (including the left recurrent laryngeal nerve). Finally, there are cardiac nerves and lymph nodes.
Inferior Mediastinum:
It is located below the transverse thoracic plane. This area is further divided into different sections for better organization.
Anterior Mediastinum:
Smallest part, in front of the pericardium.
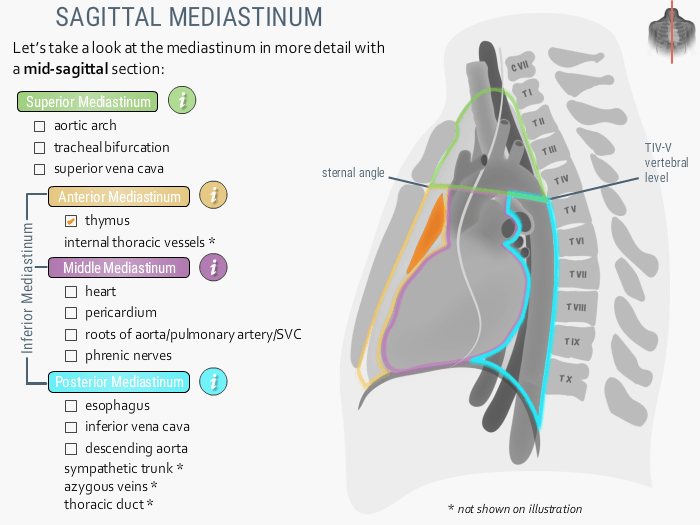
■ Borders: Transverse thoracic plane (top), diaphragm (boom), sternum body/xiphoid (front), pericardium (back), mediastinal pleura (sides).
■ Contents: Remnants of the thymus gland, especially in children. It also includes fat, connective tissue, lymph nodes, and sternopericardial ligaments. Additionally, there are branches of internal thoracic vessels.
Middle Mediastinum:
The largest part is located centrally.
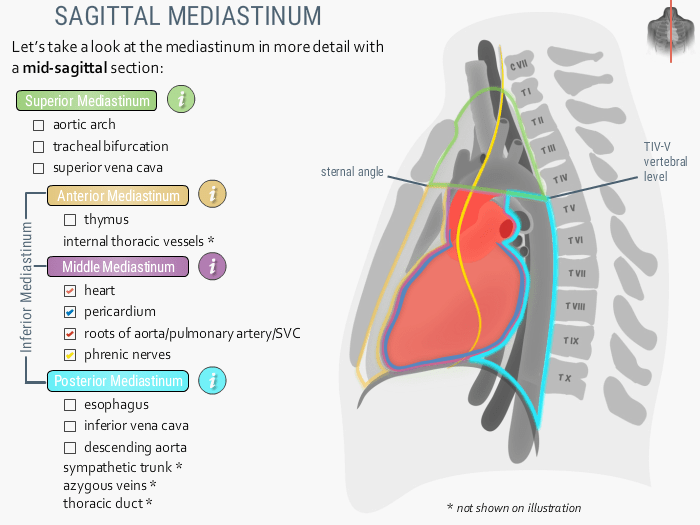
■ Borders: Transverse thoracic plane (top), diaphragm (boom), front/back of pericardium (front/back), mediastinal pleura (sides).
■ Contents: Heart enclosed within the pericardium. It includes the roots of the great vessels. These include the ascending aorta, pulmonary trunk, lower superior vena cava, and pulmonary veins. The tracheal bifurcation (carina) and main bronchi are also part of the contents. It also includes phrenic nerves. Additionally included are the cardiac plexus and tracheobronchial lymph nodes.
Posterior Mediastinum:
Located behind the pericardium.
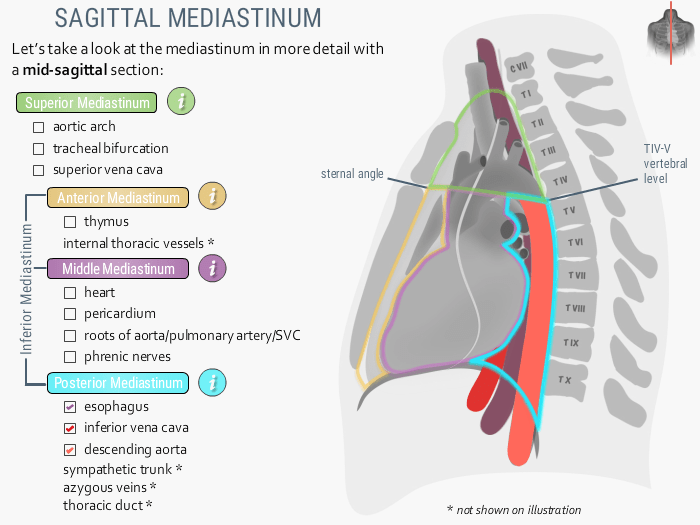
■ Borders: Transverse thoracic plane (top), diaphragm (boom), posterior pericardium (front), T5-T12 vertebrae (back), mediastinal pleura (sides).
■ Contents: Lower esophagus, descending thoracic aorta, azygos, and hemi-azygos venous systems. It also includes the thoracic duct and vagus nerves (forming esophageal plexus). Additionally, it holds sympathetic trunks, splanchnic nerves, and lymph nodes.
● Alternative Classification: The four-compartment model is traditional. A newer three-compartment model (prevascular, visceral, paravertebral) is based on cross-sectional imaging, like CT scans. This model is also used clinically.
● Key Structures (Overall): Includes the heart. It also includes the great vessels (aorta, pulmonary trunk, vena cavae). Additionally, there are the trachea, esophagus, thymus, and thoracic duct. Various important nerves (phrenic, vagus, cardiac) are present, along with numerous lymph nodes. It acts as a vital conduit or “railroad station” for structures passing between the neck and abdomen.
● Physiological Functions:
Protection: The mediastinum provides a safe space for vital organs like the heart, trachea, and esophagus. This space is supported by cushioning fat and connective tissue. The sternum protects it in the front. The spine protects it in the back. This ensures the safety of these structures. The fibrous pericardium adds further protection.
○ Passageway: Allows transit of structures like the esophagus, trachea, nerves, and major blood vessels between different body regions.
○ Support & Coordination: Organizes organs for coordinated cardiovascular, respiratory, and digestive functions. Fay/connective tissues offer cushioning and support.
○ Immune Role: Houses lymph nodes vital for immune surveillance in the thorax.
○ Interaction with Chest Wall: Conditions like pectus excavatum/carinatum show how chest wall shape affects the mediastinum and heart/lung function.
Anatomy of the Pericardium
● Definition & Location:
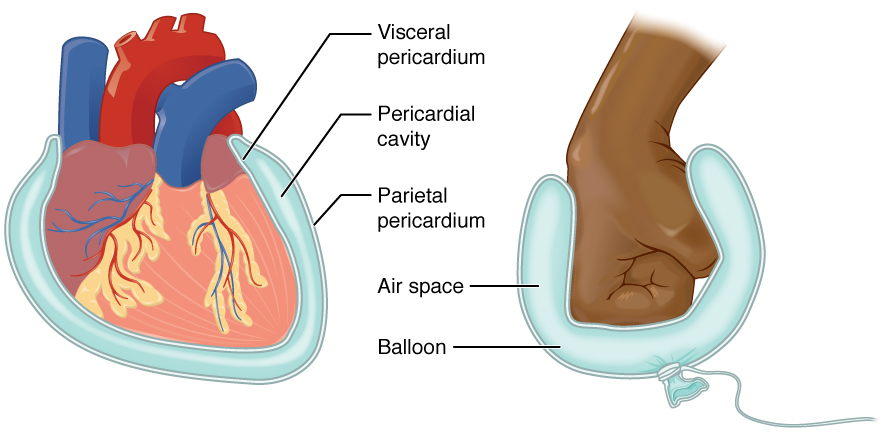
The pericardium is a protective sac surrounding the heart and the roots of the great vessels. It is located in the middle mediastinum, behind the sternum, and between the T5 and T8 vertebrae. It directly covers the heart’s outer surface. Its location highlights the organized structure within the chest.
● Layers: Consists of two main layers:
○ Fibrous Pericardium (Outer): is a tough, dense layer of connective tissue that surrounds and protects the heart.
■ Attachments: It connects with the diaphragm’s central tendon via the pericardiophrenic ligament. It also fuses with the outer layer, known as the tunica adventitia, of the great vessels. The fibrous pericardium is attached to the sternum by the sternopericardial ligaments.
■ Property: Relatively inelastic, preventing rapid overfilling of the heart.
○ Serous Pericardium (Inner): Thin, double-layered membrane.
■ Parietal Layer: Lines the inner surface of the fibrous pericardium, fused to it.
■ Visceral Layer (Epicardium): Directly covers the heart’s outer surface and roots of great vessels.
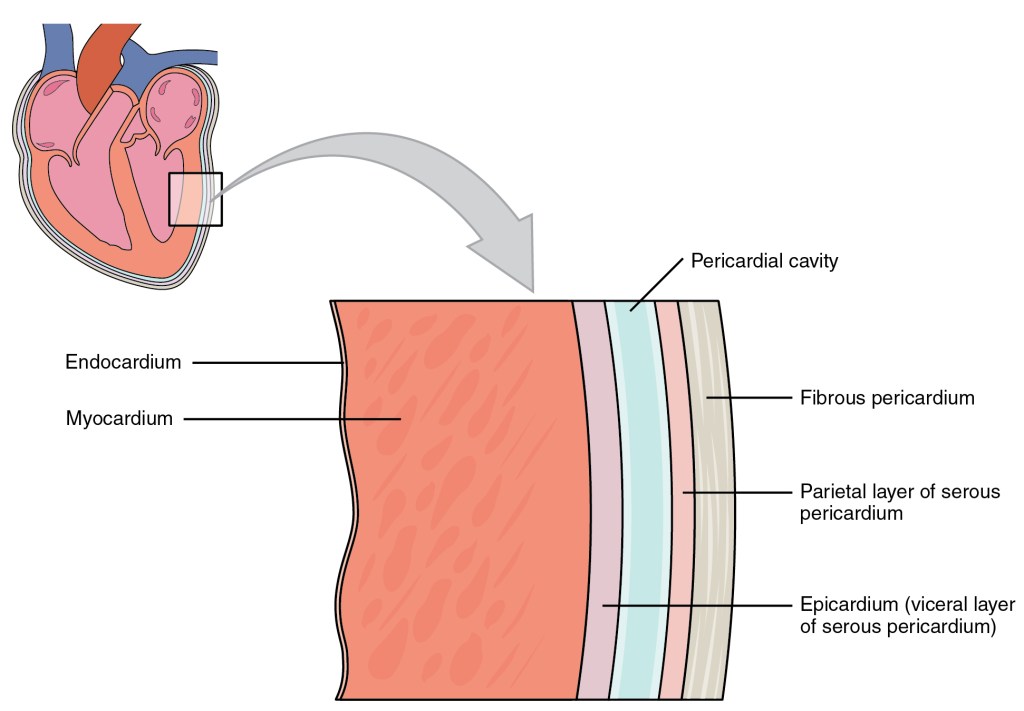
■ Pericardial Cavity: Potential space between parietal and visceral layers, normally containing 15-50 mL of lubricating serous fluid.
● Pericardial Sinuses and Recesses: Reflections of the serous pericardium form spaces:
○ Transverse Pericardial Sinus: Passage behind the aorta and pulmonary trunk, in front of the superior vena cava. It is clinically significant as it allows surgeons to clamp the major arteries during heart surgery.
○ Oblique Pericardial Sinus: is a pocket behind the left atrium, situated between the pulmonary veins. Allows space for left atrial expansion.
○ Other smaller recesses exist; recognizing these normal structures on imaging is important to avoid misdiagnosis.
● Structure & Function Link: The strong brous layer and lubricating serous layer show how structure enables function.
● Physiological Functions:
○ Physical Barrier: Protects the heart from nearby infections (e.g., from the lungs) and physical trauma.
○ Prevents Overloading: The inelastic fibrous layer limits acute heart dilation, especially with sudden volume increases, maintaining optimal size.
○ Reduces Friction: Serous fluid allows smooth, unimpeded heart movement during contraction and relaxation.
○ Fixes the Heart: Anchors the heart to the diaphragm, sternum, and great vessels, limiting excessive movement.
○ Influences Cardiac Mechanics: Contributes to heart chamber pressure-volume relationships and helps maintain the ventricle geometry.
○ Force Equalization: This may help equalize hydrostatic, inertial, and gravitational forces acting on the heart.
Clinical Significance and Common Disorders
● Clinical Relevance of Mediastinum: A critical area due to its vital contents.
○ Mediastinal Masses: Benign/malignant tumors, cysts, and lymph node enlargement can occur. Location is key for diagnosis. Specific examples by
location:
■ Superior: Aortic aneurysm, thymic tumors, thyroid goiters.
■ Anterior: Thymomas, lymphomas, teratomas, thyroid goiters.
■ Middle: The middle mediastinum can show lymphadenopathy (often from lung cancer) and conditions like bronchogenic or pericardial cysts.
■ Posterior: Neurogenic tumors (schwannomas, neurofibromas), esophageal cancer, diaphragmatic hernias, aortic dissection.
○ Mediastinitis: Serious inflammation of mediastinal tissues, oen post-cardiac surgery or from esophageal perforation.
○ Pneumomediastinum: Air in the mediastinum, from lung rupture or trauma.
○ Mediastinal Widening: Seen on chest X-ray, can indicate serious issues like aortic dissection or hemorrhage, prompting further investigation.
○ Trauma: Chest trauma can harm major vessels and nerves located within the mediastinum.
● Clinical Relevance of Pericardium: Disorders can have serious consequences due to the heart’s enclosure.
○ Pericarditis: This inflammation is often caused by infections or autoimmune diseases. It presents with chest pain. Sometimes, it produces a specific sound called a pericardial friction rub. This sound can be heard with a stethoscope. The pain can be referred to the shoulder through the phrenic nerve.
○ Pericardial Effusion: Pericardial effusion is the buildup of excess fluid in the pericardial cavity.
○ Cardiac Tamponade: A life-threatening condition where effusion fluid compresses the heart, impairing its ability to pump blood. Requires immediate drainage.
○ Constrictive Pericarditis: Chronic inflammation causes the pericardium to thicken. It leads to scarring and calcification. These changes restrict the heart’s ability to fill with blood during relaxation (diastole).
○ Pericardial Cysts: Rare, benign fluid-filled sacs near the pericardium.
○ Congenital Absence: It is a rare condition where individuals are born without part or all of the pericardium. This condition is usually asymptomatic. Nevertheless, it can be relevant in certain situations.
In conclusion, the mediastinum is the central compartment of the chest. It is divided into sections that protect vital organs. It also serves as a key passageway. The pericardium, within the middle mediastinum, acts as a protective sac for the heart, reducing friction and anchoring it. Understanding their anatomy and functions is vital for diagnosing and treating related conditions.


Leave a comment